Abstract

Introduction: Pain in sickle cell disease (SCD) starts as episodes of recurrent pain and progresses to chronic pain with age. Pain is typically treated with opioids which are often insufficient. One reason for this may be that opioids likely do not effectively treat neuropathic or inflammatory pain in SCD. Cannabinoids, such as marijuana, alleviate neuropathic pain and reduce inflammation. Our SCD patients report marijuana improves their pain and studies in murine models of SCD show cannabinoids reduce mast cell activation, inflammation, and hyperalgesia. Medical marijuana is now legal in 28 states and 4 of them list SCD as a qualifying condition. However, there are minimal data on the use of marijuana in SCD. Thus, we performed a pilot study of adults with SCD who use daily marijuana. Our hypothesis was that daily marijuana users would have worse pain scores from non-daily users which drives their drug use. Our secondary hypotheses were that daily marijuana users may have decreased levels of opioid use, hospital utilization, quality of life measures (QoL) or inflammation.
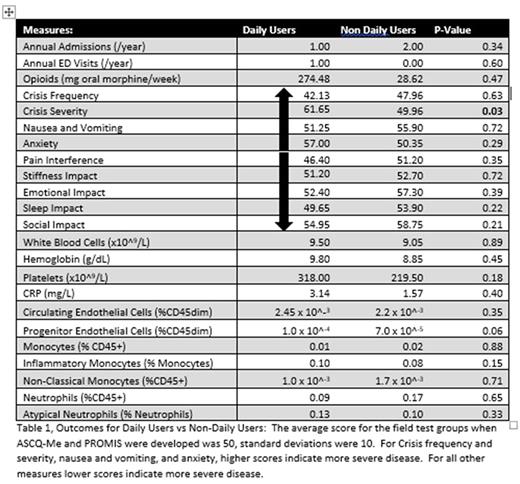
Methods: We conducted a cross-sectional pilot study of adults living with SCD who do and do not use daily marijuana. Subjects were enrolled at scheduled clinic visits, any subject not at their heathy baseline was excluded. Subjects were asked if they had used marijuana in the past 30 days, reasons for use, and rate of use. Subjects who reported daily use were compared to those who used less often or reported no marijuana use. Our primary outcome was pain as defined by Adult Sickle Cell Quality of Life measurement information system (ASCQ-Me) pain domains. ASCQ-Me has separate domains for pain crisis frequency, pain crisis severity, and 7-day pain interference which allows for measurement of both crisis pain and chronic pain. Our secondary outcomes were differences in hospital utilization, opioid use, QoL measures included in ASCQ-ME: sleep, stiffness, social impact and emotional impact, Patient Reported Outcome Measurement Information System domains for nausea and anxiety, and inflammation as demonstrated by WBC and platelet counts, C reactive protein (CRP), markers of mast cell and neutrophil activation and endothelial damage. Hospital utilization (total annual admissions and emergency room visits) was assessed by medical record review over a one-year period (1/1/2016 to 12/31/2016). Weekly opioid use was estimated by review of dispensed prescriptions using the Connecticut Prescription Monitoring Program converted into average weekly oral morphine equivalents. Flow cytometry was performed for levels of: neutrophils and activated neutrophils, monocytes, non-classical and inflammatory monocytes, circulating endothelial cells (CECs) and endothelial progenitor cells (EPCs). The R statistical software program was used to perform t-tests and Wilcoxon rank-sum tests where normality was not met to compare daily users to non-daily users. Significance was set at p<0.05.
Results: We enrolled 29 subjects,16 (55%) of whom reported marijuana use in the past 30 days and of those 6 (21%) reported daily marijuana use. Pain relief was endorsed as a reason for marijuana use in 93% of users and 100% of daily users. There was no difference in mean age (32.0 SD 8.6 vs 32.4 SD 12.6 years p=1.0) or gender (% female: 67 vs 52% p=0.7) between groups. Daily marijuana users had higher pain crisis severity scores (61.7 vs 50.0 p=0.03). There was no significant difference in scores for pain crisis frequency, pain interference, or other QoL measures (Table). Daily users had similar median annual admissions and emergency room visits to non-daily users (1.0 (IQR 0.25-1.0) vs 2.0 (IQR 0 - 5.0) admissions p=0.3; 1.0 (IQR 0.25-1.75) vs 0 (IQR 0-1.5) ED visits p=0.6) and used similar doses of weekly opioids (274.5 [IQR 91.5-3447.9] vs 28.6 [IQR 3.03-135.6] mg weekly po morphine equivalents p=0.5). There were no differences in CRP, CBC, CECs or EPCs, or in levels of all neutrophils and monocytes types.
Conclusion: In our pilot study, we found daily marijuana users reported more severe pain crisis, but had similar rates of hospital utilization and similar amounts of opioids dispensed. We posit that patients with more severe pain crisis may use daily marijuana to effectively treat their pain allowing them to have similar hospital and opioid utilization to those with less severe pain. Larger prospective studies should be performed to test these hypotheses.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal